|
This condition results from wearing of the joint cartilage between the humeral head and the socket. It does not usually occur as a result of overexertion, as is the case with arthrosis in the hip or knee, for example, but as a result of a disruption in the nutrition of the cartilage. Major rotator cuff lesions can impede the nutrition of the entire joint cartilage and ultimately lead to what is known as "defect arthropathy". Put simply, this means that joint wear (arthrosis) occurs as a result of a major defect of the rotator cuff (tendon cuff around the head of the shoulder). The cartilage is used up, the bones of the humeral head and the socket rub against each other without the protection of this shock-absorbing joint cartilage. This leads to pain and restriction of movement. Since people in our culture are now living longer thanks to advances in medicine and a good diet, we increasingly have to deal with the consequences of ageing. Accordingly arthrosis in the joints and appropriate treatment options are gaining in importance. Joint replacement operations have now become a routine part of maintaining quality of life, and are likely to remain so unless it becomes possible in the future to use genetic engineering methods to transplant and regenerate large quantities of joint cartilage which can then be used to preserve the natural joint. This is no utopian dream of the future but is already a practical reality, albeit on a small scale.
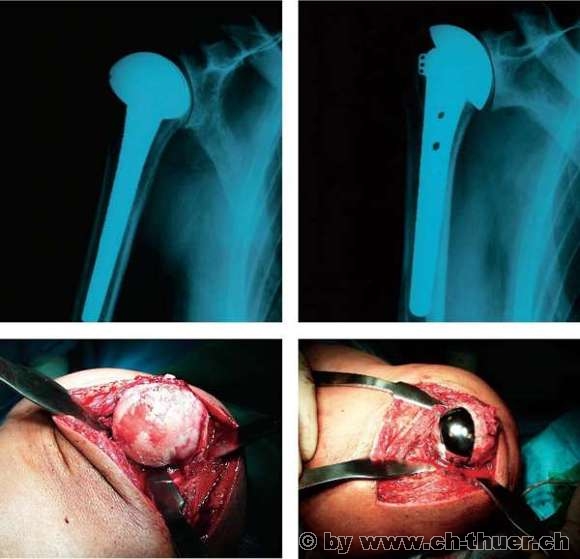
Whereas artificial hips and knees have reached a highly advanced stage of development and have been standardised, the same is not completely true of shoulder implants. Since the most important part of the shoulder is not the joint itself, but the mobile covering of soft tissue (rotator cuff), simply replacing the joint surfaces is often not satisfactory on its own. The main aim, of course, is to provide freedom from pain, but most patients also want to restore the mobility and strength of their shoulder. In cases of advanced arthrosis however, the RC components are not infrequently so badly damaged, or even completely missing, that restoring full mobility and strength becomes a matter of luck and is not always achievable despite intensive post-operation strengthening exercises. This suggests that joint replacement surgery should not be deferred until the point where all structures are destroyed, but should be carried out when the patient is suffering badly and the changes have not yet become too advanced. A shoulder prosthesis implanted by a capable surgeon will yield good results at this stage.
Follow-up management will therefore always be geared to the surrounding structures (rotator cuff), which will also need to be treated at the same time. The prosthesis itself can be subjected to loading from the start. An implant rarely needs to be changed nowadays because of loosening, which usually affects the socket component only. For this reason, many shoulder surgeons do not always replace the socket to begin with, preferring to replace the humeral head alone, particularly if major RC defects are also present.
Während die Hüft- und Kniegelenksprothetik bereits sehr fortgeschritten sind und eigentlich standartisiert, trifft dies noch nicht ganz auf den Schultergelenksersatz zu. Da das Wichtigste an der Schulter nicht das Gelenk selbst ist, sondern der bewegende Weichteilmantel (Rotatorenmanschette), ist auch der alleinige Ersatz der Gelenkflächen häufig nicht befriedigend. Das Hauptziel ist sicher die Schmerzbefreiung, aber die meisten Patienten möchten auch die Beweglichkeit und Kraft wiederhergestellt haben. Bei fortgeschrittenen Arthrosen sind aber nicht selten die RM-Anteile so schlecht oder sogar vollständig fehlend, so dass die volle Beweglichkeit und Kraft eine Glückssache wird. Trotz intensivem Aufbautraining nach der Operation sind diese Wünsche und Ziele nicht immer erreichbar. Dies spricht dafür, dass mit einer Gelenksersatzoperation nicht abgewartet werden sollte, bis alle Strukturen zerstört sind, sondern dann durchgeführt werden soll, wenn der Leidensdruck gross ist und Veränderungen noch nicht zu fortgeschritten sind. Eine Schultergelenksprothese in diesem Stadium geben nämlich in guter Hand gute Resultate.
Die Nachbehandlung richtet sich deswegen immer nach den umgebenden Strukturen (Rotatorenmanschette), welche mitbehandelt werden müssen. Die Prothese selbst wäre schon primär belastbar. Ein Prothesenwechel wegen Lockerung ist heute sehr selten und betrifft meistens nur die Pfannenkomponente, weswegen viele Schulterchirurgen die Pfanne nicht immer schon von anfang an ersetzen. Vor allem bei gleichzeitig grossen RM-Defekten wird heute der alleinige Gelenkkopfersatz vorgezogen.
|