|
PHS: periarthritis humeroscapularis or, in lay terms, soft tissue inflammation of the shoulder
This diagnosis is a melting pot that actually covers all types of rheumatic inflammation of the shoulder and all soft tissue disorders of the shoulder without a more specific diagnosis. Although modern medicine has managed to extract many individual disease complexes from this melting pot and defined each as a separate clinical condition, a number of pain complexes are still covered by PHS. Future research and development will succeed in identifying several more such individual illnesses so that appropriate treatment can ultimately be provided. One such inflammatory disorder is e.g.:
Frozen shoulder: an inflammatory swelling and contraction of the joint capsule that occurs spontaneously or after an accident and that ends in a severe, painful stiffening of the shoulder.
Tendinitis calcarea of the rotator cuff
(tendonitis with calcium deposition)
In this condition, calcium is deposited in the tendon plate of the rotator cuff, usually as the result of rheumatic inflammation or trauma. We know that this phenomenon also affects other tendons. In some patients this calcium deposition can lead to severe inflammatory flare-ups. A not infrequent consequence is the need for emergency medical consultations and the initiation of immediate treatment. Occasionally, surgery may be required at an early stage. In other patients this disorder follows a more chronic course involving uncharacteristic shoulder pain or periodic painful episodes followed by very long symptom-free phases. Not infrequently, these calcium deposits are also spotted as a chance finding on x-rays. This tendon calcification can lead to a bottleneck situation beneath the acromion. Alternatively, the bursa located above the tendon may swell up to such an extent that insufficient space is available beneath the acromion for the joint to slide normally, resulting in a severe pain syndrome in the shoulder. The initial treatment consists of measures to reduce the swelling, e.g. by the application of cold, anti-inflammatory drugs and gentle physiotherapy.
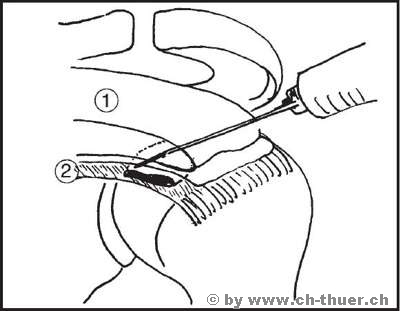
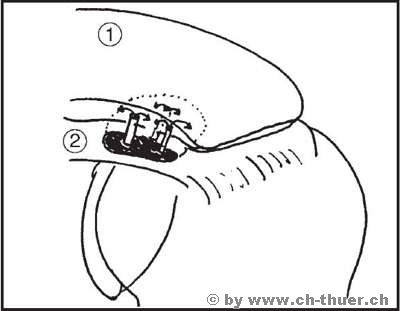
At a later stage, needling the calcium focus can prove successful, provided the focus is not too large. The drawing below illustrates the idea behind this procedure and its application.
Procedure: Under x-ray image intensifier control, the doctor looks for the site of calcium deposition and injects the local anaesthetic. The calcium deposit is now perforated several times through the bursa with a wide-bore needle, thereby creating several connecting points between the calcium in the tendon and the bursa. In many cases, cylinders of calcium can be punched out by aspiration with the syringe. Finally, the bursa is filled with a lot of fluid and some cortisone. Over the following days and weeks, the calcium is liquefied and flows out into the bursa. The purpose of adding cortisone to the fluid is to avoid severe bursitis. While most cases of calcification can be cured by this procedure, this does not mean that it will not recur in the future. Surgical removal is recommended for major calcium deposits larger than 1-2 cm in diameter. During this procedure the acromial space can be widened at the same time as the calcium is removed, which generally results in lasting freedom from pain.
|